The Crucial Role of Employee Wellbeing Programs in Healthcare
- Patricia Maris

- Apr 9, 2025
- 7 min read
Updated: Jun 10, 2025
Introduction
Healthcare is not only about patients; it's about the people who care for them. When a healthcare professional leaves, the effects are staggering. Consider a general practitioner at a busy clinic in Melbourne or an experienced nurse at a mid-sized hospital in the U.S. Their departure leads to more than just an empty seat; it impacts recruitment costs, training expenses, workflow disruptions, and lost patient trust.
The numbers are alarming. Recruitment can cost AUD 50,000 in Melbourne or up to $90,000 in the U.S. Six-figure losses in revenue often follow. This isn't just a staffing crisis; it's a crisis of sustainability.
What if we could prevent this situation? Investing in employee wellbeing programs offers a robust strategy. It helps retain talent, reduces burnout, and strengthens healthcare teams. This isn't just about cost savings; it's about enhancing lives. We need to shift our focus from damage control to proactive care for patients and those who serve them.
I Financial Costs
Addressing the loss of a General Practitioner (GP) in Melbourne at a clinic with 10-15 employees alongside a nurse in a mid-sized U.S. hospital reveals systemic challenges in healthcare. Here’s how the costs breakdown:
Recruitment and Hiring Expenses:
Hiring a GP in a Melbourne clinic can cost AUD 30,000–50,000, which includes advertising, recruitment agency fees, and onboarding.
The cost of hiring an experienced nurse in the U.S. ranges from $52,000–$90,000, accounting for relocation packages or signing bonuses.
Training Costs:
GPs endure extensive training for patient relationships, interrupting workflows and incurring additional costs of AUD 60,000–80,000 annually.
Training for clinical nurses, especially in specialized areas like ICU or ER, can reach $40,000–$70,000, with extra funds allocated for orientations and certifications.
Operational Disruptions:
During a GP shortage, clinics may lose annual revenue exceeding AUD 100,000 due to reduced patient appointments.
Mid-sized hospitals in the U.S. face unfilled shift penalties and overtime costs, which can lead to losses in revenue worth hundreds of thousands.
II. Emotional and Psychological Impacts on Staff
The emotional toll of losing a team member in healthcare is significant. It impacts staff morale and patient care profoundly. Both small clinics and large hospitals face unique challenges that ripple throughout their systems.
Melbourne Clinic (GP):
The intimate nature of small practices magnifies the loss. Employees may feel guilt, helplessness, or anxiety, which can further lead to burnout and staff attrition.
Patients who trust their GP might experience grief or a loss of confidence in the clinic, affecting their continuity of care.
U.S. Hospital (Nurse):
Already strained staff in hospitals feel even more pressure. This often results in increased absences and a 25-30% drop in morale.
Emotional exhaustion impacts teamwork, jeopardizing patient safety and quality within the hospital.

III. Time Investment in Rebuilding Trust
Trust is essential in healthcare yet can shatter due to staff losses. For patients with chronic or mental health conditions, rebuilding trust in a new caregiver is often lengthy and uncertain. Employees also need months or even years to regain confidence and cohesion within their teams.
Patients (GP):
Months can pass before patients trust a new GP, especially those with chronic issues who require ongoing care.
Employees:
Restoring trust among employees and the team can take over a year and requires dedicated support programs and transparent communication.

IV. Legal and Compliance Considerations
Legal and compliance challenges in healthcare extend beyond mere policies. Following a staff loss, organizations face potential liabilities and rigorous workplace safety reviews. Whether a clinic deals with claims of unsafe conditions or a hospital navigates lawsuits and audits, these challenges can strain resources.
Melbourne Clinic (GP):
Clinics face potential liability if employees claim workplace conditions contributed to the loss. Legal and compliance audits can be costly.
U.S. Hospital (Nurse):
Hospitals may face negligence lawsuits and compliance audits, driving up legal costs significantly.

V. Short-Term and Long-Term Effects
The loss of a healthcare professional sends ripples through the organization. Immediately, there’s pressure to fill gaps with temporary hires and overtime, leading to financial strain. Over time, the consequences deepen. High turnover diminishes team unity, reduces care quality, and amplifies patient dissatisfaction, further eroding a tarnished workplace reputation.
Short-Term:
Covering shifts incurs sudden financial strains and remaining employees may leave due to heightened stress.
Long-Term:
High turnover damages cohesiveness and care quality, resulting in lower patient satisfaction ratings.
Negative workplace culture discourages top talent, limiting future hiring possibilities.



VI. Strategies for Supporting Staff Morale
Supporting morale in healthcare is essential. It's not only about creating a positive workplace; it's about saving lives, retaining employees, and maintaining care quality. Initiatives like confidential employee assistance programs (EAPs) and flexible scheduling at the Melbourne Clinic aim to provide relief to remaining staff.
Similarly, U.S. Hospitals focus on wellness programs and training to rebuild trust. These proactive measures are lifesavers in an industry where stress can lead to terrible outcomes.
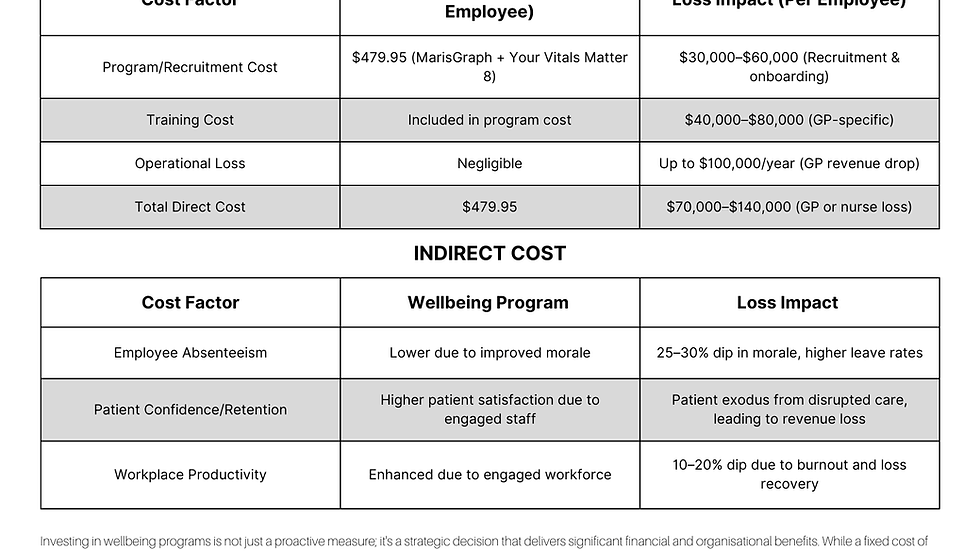
This section highlights the costs and impacts of implementing wellbeing programs such as MarisGraph and Your Vitals Matter 8. It’s crucial for healthcare organizations to adopt feasible strategies that elevate mental health, reduce stress-related losses, and enhance workforce resilience.
Melbourne Clinic:
Implement a confidential EAP to support mental health.
Offer flexible scheduling to alleviate stress.
Hold team debriefings for emotional relief.
U.S. Hospital:
Provide wellness initiatives like mindfulness sessions and gym memberships.
Train managers in trauma response and empathy.
Recognize the efforts of remaining staff through acknowledgment or awards.
VII. Recommendations for Preventative Measures
Impact Over Time (Patient Continuity) Before Wellbeing Program:
Staff burnout and disengagement strain patient-provider interactions.
Patients sense emotional detachment, diminishing trust in care.
Patient retention declines as individuals seek more attentive alternatives.
Relationships and community trust in healthcare erode.
Impact Over Time (Patient Continuity) After Wellbeing Program:
Wellbeing initiatives re-engage staff, uplifting morale and motivation.
Patient interactions are more friendly and timely.
Increased patient satisfaction leads to better retention rates.
Healthcare establishes a reputation for compassion and sustainability.
Promote Mental Health Awareness and Training:
Train the entire organization to recognize early signs of burnout and distress.
Integrate open discussions about mental health.
Balance Workloads:
Regularly assess workloads to ensure proper staffing ratios.
Implement Support Systems:
Initiate peer mentoring for new hires or those in emotionally taxing roles.
Ensure Leadership Accountability:
Create roles focused on staff wellbeing.
Maintain open feedback loops for employees to voice concerns comfortably.
This tragedy highlights our healthcare professionals' importance. By addressing these challenges proactively, we can create supportive environments that benefit both staff and the patients they serve.
Whatever support you seek, reaching out is a decisive first step. It has the potential to uplift
your mental health and transform your overall wellbeing.
VIII References:
This analysis is based on general knowledge and industry standards.
Recruitment and Training Costs:
Data on recruitment and training costs for healthcare professionals were gathered from industry averages and HR studies.
Emotional and Psychological Impacts:
Insights were derived from studies on workplace mental health and the effects of losing a colleague.
Legal and Compliance Considerations:
Information informed by workplace safety regulations in Australia and the U.S.
Strategies and Preventative Measures:
Recommendations are based on best practices in organizational psychology and employee wellness.
Disclosure Our pricing adapts over time, but we offer exclusive discounts for large groups and corporate clients to ensure exceptional value
Unlock Your Wellness Potential:
A Deep Dive into Self-Understanding with e7D-Maris Graph.

Understanding ourselves is the first step toward optimal wellbeing. I'm excited to introduce an innovative tool—the e7D-Maris Graph.
The e7D-Maris Graph is designed to evaluate your wellbeing comprehensively. It assesses eight critical pillars, providing insights into your health status.
This assessment empowers you to take control of your wellbeing, identify areas for improvement, and guide you toward your highest potential. Whether you're starting your wellness journey or seeking to refine your routine, the e7D-Maris Graph offers invaluable guidance tailored to your needs.
So, are you ready to explore your wellness journey? Here’s your chance!
Unleash Your Potential with e7D-Maris Graph Now! FREE
Take the e7D-Maris Graph test today, better understand your wellbeing, and embark on your journey toward a healthier, balanced life. Discover your strengths and areas for growth.
Your path to optimal wellness is just a click away. Uncover your wellness scores and unlock your full potential today!
To your health and success,
The e7D team.




Comments