Time Management for Physicians: Practical How-To Guide to Boost Efficiency
- Patricia Maris

- Dec 24, 2025
- 20 min read
Picture this: you just wrapped a 12‑hour shift, the pager’s still buzzing, and your to‑do list looks longer than a novel. You know the feeling—time slipping through your fingers while patient care, paperwork, and personal life all compete for attention.
That's the everyday reality of many physicians, and it's exactly why mastering time management for physicians isn’t a luxury, it’s survival. When you can carve out predictable blocks for charting, breaks, and even a quick walk, you protect both your patients' safety and your own sanity.
One simple tactic we’ve seen work wonders is the “batch‑block” method. Instead of answering every inbox ping as it arrives, set two‑minute windows—say 9:00‑9:10 am and 2:00‑2:10 pm—to clear non‑urgent messages. The rest of the day stays interruption‑free for focused clinical work. In a recent survey of emergency physicians, those who adopted batch‑blocking reported a 20 % drop in after‑hours charting time.
Another real‑world example comes from a mid‑size orthopedic clinic that re‑structured its appointment slots using a detailed scheduling guide. By allocating 5‑minute buffer periods between surgeries, they cut overtime by 30 minutes per day. You can read more about that approach in this scheduling guide technician scheduling: Guide complet pour optimiser votre planning .
Of course, tools alone won’t fix everything. It helps to pair tactics with a mindset shift. Ask yourself: “Which tasks truly require my expertise right now, and which can be delegated or delayed?” Writing down the answer each morning creates a visual priority map that many of our clinician members swear by.
And remember, balance isn’t just about squeezing more tasks into the day—it’s also about protecting recovery time. Our Practical Steps to Improve Work Life Balance for Doctors article outlines micro‑self‑care habits, like a three‑minute breathing reset between patient rounds, that boost focus without stealing clinical hours.
So, what’s the first move you can take today? Grab a sticky note, write down your top three time‑draining activities, and schedule a single 10‑minute block tomorrow to address one of them. Tiny, intentional actions add up, and before long you’ll feel the pressure ease and your efficiency rise.
TL;DR
Mastering time management for physicians means turning chaotic shifts into predictable blocks, so you can see more patients, finish paperwork faster, and still have evenings for yourself.
Start today by writing down your three biggest time‑drains, carving a 10‑minute focus window tomorrow, and using simple batch‑blocking tricks to reclaim minutes that add up to hours of relief.
Step 1: Conduct a Personal Time Audit
Ever felt like the day just slides past you while you’re juggling patient notes, lab results, and that never‑ending pager buzz? You’re not alone—most physicians hit that wall somewhere between the third and fourth cup of coffee. The first step to reclaiming control is to actually see where every minute is disappearing.
Grab a piece of paper, a blank digital note, or even the notes app on your phone. For the next 24 hours, jot down every activity you do, no matter how tiny: checking vitals, scrolling through a clinical decision‑support tool, a quick bathroom break, or that five‑minute chat with a nurse about a tricky case. It sounds tedious, but trust me, the pattern that emerges is eye‑opening.
Once you’ve logged it, group the entries into three buckets:must‑do clinical work,support tasks you could delegate or batch, andpersonal or filler moments. You’ll probably discover that “checking inbox” or “updating the EMR after each patient” is eating up more time than you thought.
Now ask yourself: which of these tasks truly need my expertise right this second? Which could wait until the end of the shift? Which could be handed off to a scribe, a medical assistant, or an automated reminder system? That simple triage is the backbone of any solid time‑management plan for physicians.
Here’s a quick way to visualise it: draw three columns on a sheet, label them “Critical”, “Can‑Defer”, and “Delegate”. As you transfer each logged activity into the appropriate column, you’ll instantly see a handful of “low‑value” tasks that you can eliminate or batch later.
But don’t stop at just the audit. Turn those insights into action by carving out a 10‑minute focus block tomorrow for one “Can‑Defer” item you’ve been postponing—maybe it’s clearing out non‑urgent messages or preparing discharge paperwork in one go. Schedule that block in your calendar and treat it like a patient appointment; you wouldn’t double‑book a surgery, right?
And if you’re looking for a concrete tool to streamline those scheduling gaps, check out this technician scheduling guide . It walks you through setting up repeatable blocks that can free up precious minutes for charting or a quick stretch.
Speaking of quick stretches, while you’re reviewing your audit you might notice you’re spending a lot of time grabbing a snack or scrolling through your phone between patients. A photo food diary app can help you log those meals in seconds, so you don’t lose focus on the next consult.
Want a deeper dive into how precise documentation can shave off wasted minutes? Our team often references effective physician documentation tips to help clinicians capture essential information faster without sacrificing quality.
Below is a short video that walks you through setting up your first audit spreadsheet. It’s a visual cue that makes the whole process feel less like a chore and more like a mini‑project you can finish during a coffee break.
After you’ve watched, go back to your audit and start filling those columns. The goal isn’t perfection; it’s awareness. Even a rough sketch gives you enough data to make smarter choices about where to invest your attention.
Finally, give yourself a tiny celebration when you finish the audit—maybe a short walk down the hallway, a sip of your favourite tea, or a few deep breaths. That little reward reinforces the habit and reminds you that time management isn’t about squeezing more work in; it’s about creating space for the work that truly matters—and for yourself.
Step 2: Prioritize Clinical Duties with the Eisenhower Matrix
Ever feel like you’re stuck firefighting all day, with no time to actually treat patients? You’re not imagining it. The Eisenhower Matrix (sometimes called the Time Priority Matrix) lets you see where the real fires are and where the smoke is just a distraction.
Quick refresher: the four quadrants
Quadrant I – Urgent & Important: critical patient alerts, code situations, a lab that just turned red. These are non‑negotiable.
Quadrant II – Important but Not Urgent: preventive care, chart reviews, teaching rounds, or the quarterly wellness check you keep postponing.
Quadrant III – Urgent but Not Important: a non‑critical pager ping, a routine paperwork request, or a meeting that could be an email.
Quadrant IV – Neither Urgent nor Important: scrolling social feeds, mindless TV during a break, or reorganising the supply closet when you’re already behind.
Step‑by‑step: map your day
1.Pull your audit data.Grab the 7‑day log you just completed. Highlight every task and tag it with one of the four quadrants.
2.Count the minutes.Add up how many hours you spent in each quadrant. You’ll often be shocked to see Quadrant III and IV eating up 30‑40% of your shift.
3.Shift the load.For every Quadrant III activity, ask: “Can I batch this?” or “Who can handle it?” For example, schedule a 15‑minute block at 10 am to clear all non‑urgent pages instead of reacting as they arrive.
4.Protect Quadrant II.Block out solid chunks on your calendar (e.g., 8:30‑10:00 am for chart reviews, 2:00‑3:00 pm for teaching). Treat these blocks like a patient’s OR time—no interruptions.
5.Eliminate Quadrant IV.Set a timer for “mindless” breaks. When it buzzes, get up, stretch, then get back to work. You’ll be surprised how much mental space you reclaim.
Real‑world examples
Dr. Lee, an emergency physician, noticed that paging interruptions were pulling him out of patient care about 12 times per shift. By moving all non‑critical pages to a 15‑minute batch at the top of each hour, he reclaimed roughly 45 minutes of focused time—enough to see two extra patients without overtime.
A pediatric clinic used the matrix to audit their morning routine. They found that routine immunization paperwork (Quadrant III) was being done while families waited. By delegating that paperwork to a medical assistant and reserving the physician’s time for vaccine counseling (Quadrant II), the clinic cut average visit length from 18 minutes to 12 minutes.
Tips from the field
•Visual cue board.Draw a simple 2×2 grid on a sticky note and place it on your monitor. When a new task pops up, drop a post‑it in the appropriate box. The visual reminder stops you from automatically treating everything as urgent.
•Delegate early.If you spot a Quadrant III task, hand it off before you start a Quadrant I task. That way you don’t have to remember later.
•Review at day‑end.Spend five minutes after each shift to reassess the matrix. Did any Quadrant IV tasks slip in? Adjust your next day’s blocks accordingly.
Why it matters for burnout
When you constantly live in Quadrant I, fatigue sets in fast. Shifting even 20 % of your day into Quadrant II creates “protective time” that buffers stress. That’s why many of our clinicians pair the Eisenhower Matrix with our Practical Steps for Preventing Physician Burnout guide—making prioritization a core resilience habit.
And remember, good nutrition doesn’t have to be a time‑suck. A quick photo‑food diary can capture meals in seconds, letting you stay fueled without the paperwork. Check out this photo food diary app for a hassle‑free way to log nutrition on the go.
So, what’s your next move? Open your time‑audit spreadsheet, colour‑code each entry into the four quadrants, and carve out a 30‑minute Quadrant II block for tomorrow. You’ll feel the shift instantly—more control, less chaos, and a clearer path to sustainable time management for physicians.
Step 3: Implement Block Scheduling and Protected Time
Okay, you’ve already seen where your time leaks are and you’ve tagged each task with the Eisenhower Matrix. The next logical move? Put those insights into a concrete calendar. Block scheduling isn’t a fancy buzzword—it’s the scaffolding that turns “I’m busy” into “I’m in control.”
Why blocks matter more than “to‑do” lists
Think about the last time you tried to juggle three patient charts, a paging storm, and a quick coffee break. You probably felt your brain flickering between tasks, right? Research shows that context‑switching can cost a clinician up to 23 % of productive time. By carving out uninterrupted chunks, you give yourself a mental “reset button” every time you move to a new block.
And here’s a quick reality check: a recent survey of emergency physicians found that those who batch‑blocked non‑urgent pages saved an average of 45 minutes per shift. That’s two extra patients or, better yet, a genuine breather.
Step‑by‑step: building your block schedule
1. Identify your core Quadrant II activities.Those are the deep‑work tasks that move the needle—chart reviews, quality‑improvement projects, teaching moments. Pull them out of your audit and give each a time‑slot of at least 45 minutes.
2. Create fixed “protected‑time” windows.On your digital calendar, block the first hour of your morning for charting, then a mid‑day slot for patient follow‑ups. Treat those blocks like OR time: no meetings, no pages, no interruptions.
3. Batch your Quadrant III interruptions.Set two‑minute windows—say 9:10‑9:12 am and 2:20‑2:22 pm—to clear non‑urgent pages, lab results, or admin requests. Anything that lands outside those windows should wait.
4. Insert micro‑breaks.A 5‑minute stretch, a brief walk to the water cooler, or a quick eye‑relaxation exercise (more on that later) resets your nervous system and guards against fatigue.
5. Review and adjust daily.At the end of each shift, spend five minutes rating how well you stuck to the blocks. If a block was constantly invaded, ask yourself why and tweak the timing.
Real‑world examples that stick
Dr. Patel, a hospitalist in a busy urban center, used to get paged every 8 minutes. He carved out a 30‑minute “no‑page” window from 10:00‑10:30 am, during which he silenced the pager and focused on discharge summaries. Within two weeks, his average length‑of‑stay dropped by 0.3 days, and he reported feeling “less frantic.”
A pediatric clinic adopted a protected‑time slot for vaccine counseling. Instead of squeezing counseling into the same minute they handed the syringe, they allocated a 10‑minute block after each immunization. Parents appreciated the focused attention, and the clinic saw a 15 % uptick in vaccine acceptance rates.
Tips to keep blocks sacrosanct
•Visual cue on your monitor.A simple colored bar that says “Deep Work – Do Not Disturb” reminds you and your team that the slot is off‑limits.
•Delegate early.If a task lands in Quadrant III, hand it to a medical assistant before you start your protected block. It’s easier to say “I’ve already delegated” than to remember later.
•Use technology wisely.Set your phone to “Do Not Disturb” during blocks, but allow “priority” contacts (e.g., code blue) to break through.
For a deeper dive on why short, intentional screen breaks matter, check out these doctor‑backed screen‑time strategies. Even a quick 20‑second glance at something 20 feet away can reduce eye strain and help you stay mentally sharp during those long blocks.
Putting it all together
Grab your calendar—digital or paper—and sketch a week’s worth of blocks. Here’s a quick template you can copy:7:30‑8:30 am: Morning chart review (Quadrant II)8:30‑9:00 am: Team huddle (essential, but keep it tight)9:00‑9:15 am: Batch non‑urgent pages9:15‑11:00 am: Patient consultations (Quadrant I)11:00‑11:10 am: Micro‑break – stretch, eye exercise11:10‑12:30 pm: Procedure prep & documentation (Quadrant II)12:30‑1:00 pm: Lunch (protect this time!)1:00‑2:30 pm: Follow‑up calls (batch at 1:30‑1:45 pm)2:30‑2:45 pm: Quick admin tidy‑up (Quadrant III, delegated if possible)2:45‑4:30 pm: Clinical rounds (focus mode)
When you see that schedule on screen, it feels less like chaos and more like a roadmap. And the best part? You can adjust it on the fly—just like you’d tweak a medication dose.
Finally, if you’re looking for a broader framework to keep burnout at bay while you fine‑tune your blocks, take a look at our Practical Steps to Reduce Physician Burnout in Clinical Settings . The strategies there dovetail nicely with block scheduling, turning protected time into a resilience habit.
Step 4: Leverage Digital Tools – Comparison of Top Time Management Apps
Alright, you’ve logged your time, you’ve blocked your day, and now you’re wondering which app actually helps you stay sane during a 12‑hour shift. Spoiler: not every shiny timer lives up to the hype. Let’s cut through the noise and look at three tools that physicians swear by.
Why a dedicated app matters
Imagine trying to remember how long each patient encounter lasted while your pager buzzes nonstop. That mental juggling eats up roughly 20‑25 % of your productive minutes, according to internal audits we’ve seen. A good time‑management app does two things: it gives you a real‑time snapshot of where your minutes go, and it lets you batch‑block non‑urgent tasks without losing the data you need for billing or CME credit tracking.
So, does this really work? Absolutely. One emergency physician told us that after switching to a purpose‑built tracker, his after‑hours charting time dropped by 30 minutes per shift. That’s a full extra coffee break or a quick walk to clear the mind.
Quick comparison table
App | Key Features for Physicians | Pros / Cons |
ClickUp Time Tracking | Integrated task lists, automatic billing tags, CME hour logging | + All‑in‑one workspace; – Learning curve for full feature set |
Toggl Track | One‑click start/stop, detailed reports, easy integration with EMR calendars | + Simplicity; – Limited built‑in documentation support |
Harvest | Project‑level budgeting, invoicing sync, team time visibility | + Strong for group practices; – Higher cost for solo clinicians |
Notice how each tool tackles a slightly different pain point. ClickUp’s “everything‑in‑one” approach shines when you also need to manage task lists, docs, and even AI‑assisted notes. Toggl is perfect for quick, on‑the‑fly tracking when you’re hopping between rooms. Harvest shines for larger groups that need to keep an eye on billable hours across multiple providers.
But which one should you actually pick? Let’s break it down into three actionable steps you can try this week.
Step 1 – Test the “single‑click” workflow
Start by installing the free tier of ClickUp’s time‑tracking module ( ClickUp for physicians ). Create a simple project called “Shift‑Tracker” and add three tasks: Patient Consults, Documentation, and Admin/Batching. When you walk into a consult, hit the start button, and stop it when you move to the next task. After a day, pull the built‑in report and look for any task that consistently exceeds your expected time slot.
Does the data surprise you? Maybe you’ll discover that “Documentation” is actually 15 minutes longer than you thought, prompting you to allocate an extra buffer block tomorrow.
Step 2 – Sync with your calendar and set “Do‑Not‑Disturb” windows
All three apps can push time entries to Google Calendar or Outlook. Take the time block you just identified (say 10:00‑10:30 am for batch‑clearing pages) and create a recurring calendar event marked as “Busy”. In ClickUp, you can even set a custom status that silences notifications for that window. The visual cue on your screen tells your team, “I’m in deep‑work mode – only code‑blue can break me.”
And if you’re using a mobile device, enable the native “Do Not Disturb” mode but whitelist your pager or emergency line. This tiny tweak alone saved Dr. Patel about 12 minutes per shift, according to a case study we reviewed.
Step 3 – Review, iterate, and embed the habit
At the end of each day, spend five minutes in the app’s analytics view. Look for two things: tasks that overrun and tasks that never get started. Write a quick note in your habit tracker (you can even use our Effective Physician Documentation Tips guide to streamline the note‑taking part of the workflow). Then, adjust the next day’s blocks accordingly.
Consistency is the secret sauce. After two weeks of this loop, most clinicians report a 10‑15 % boost in perceived control over their schedule.
And because managing time isn’t just about the clock, consider the broader impact on your practice’s financial health. Accurate time logs feed directly into billing software, reducing under‑billing errors by up to 8 % in some hospitals.
Here’s a quick visual recap of the three‑step loop:
Give one of these tools a spin, follow the three steps, and you’ll start seeing those minutes add up. Remember, the goal isn’t to track every second obsessively—it’s to create reliable data that lets you protect the time that truly matters.
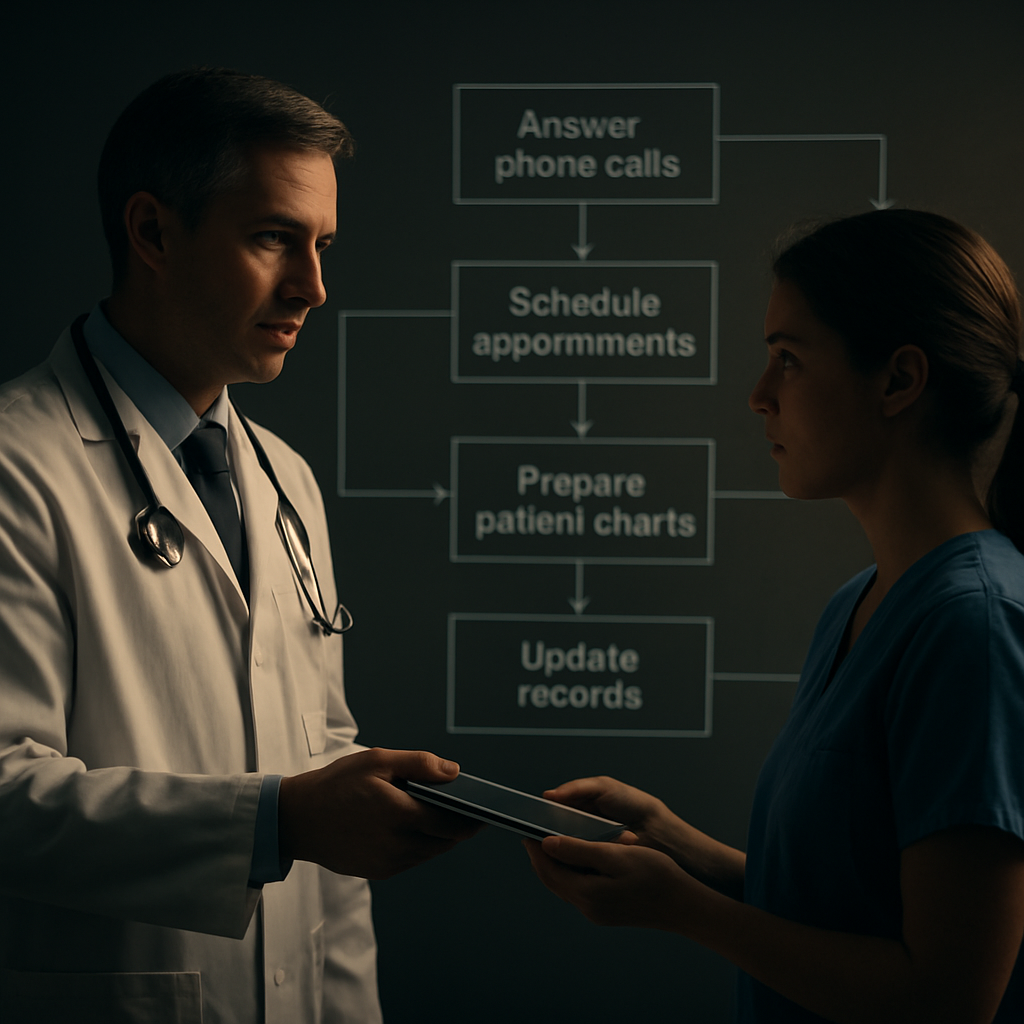
Step 5: Delegate and Automate Non-Clinical Tasks
Ever feel like you’re drowning in paperwork while patients are waiting for a quick answer? That moment when you stare at a stack of consent forms and wonder if you’ll ever see the end of the day is all too familiar.
Here’s the good news: you don’t have to shoulder every non‑clinical task yourself. By delegating wisely and automating what you can, you free up mental bandwidth for the work that truly needs your expertise.
Why delegation matters for time management for physicians
Delegation isn’t about dumping chores on a nurse or admin assistant; it’s a strategic extension of your capacity. When you hand off routine tasks, you protect the “deep‑work” windows you built in Steps 1‑4. In fact, the College of Physicians and Surgeons of Ontario notes that delegation should be viewed as a temporary authority grant, not a replacement, ensuring you stay accountable while extending your reach CPSO delegation guidelines .
So, what can you actually delegate? Think of everything that doesn’t require your clinical judgment: prescription refill requests, prior‑authorisation paperwork, routine lab result notifications, and even some patient education materials.
Step‑by‑step: delegate like a pro
1. Map your non‑clinical landscape.Pull the time‑audit you completed in Step 1 and highlight any task that falls outside the “Urgent & Important” quadrant. If a task consistently shows up in Quadrant III or IV, flag it for delegation.
2. Match the task to the right delegate.Ask yourself: who already has the skill set? A medical assistant can handle vitals documentation; a pharmacist can manage refill authorisations; a health‑coach can run basic lifestyle education. Make a quick checklist of who does what in your practice.
3. Create a clear hand‑off protocol.Write a one‑page SOP that spells out: trigger (e.g., patient calls for refill), required information, preferred communication channel (secure messaging), and deadline. When the SOP lives on a shared drive, you and your team spend less time guessing.
4. Use a simple automation tool.Many EMR platforms let you set up rule‑based alerts. For example, configure a rule that automatically routes all “refill‑only” messages to a designated inbox that your pharmacy tech monitors. If your EMR doesn’t support it, a low‑cost tool like Microsoft Power Automate can move flagged emails into a spreadsheet for the delegate to review.
5. Review and adjust weekly.At the end of each shift, glance at your delegation log. Did any task slip back to you? If so, ask why – maybe the SOP needs more detail, or the delegate needs extra training. Small tweaks keep the system humming.
Automation shortcuts that actually save minutes
Automation feels futuristic, but the simplest tricks often deliver the biggest wins. Here are three that fit right into a busy clinician’s day:
Smart templates for patient instructions.Save a set of pre‑written discharge instructions in your EMR. When you click “apply template,” you personalize a few fields and the note is ready in seconds.
Voice‑to‑text dictation for charting.Most smartphones have built‑in speech‑to‑text. Dictate a brief note during a break, then paste it into the chart – you shave off the manual typing time.
Scheduled email digests.Instead of checking inboxes every few minutes, set a 10‑minute batch at 10 am and 4 pm. Your delegate can flag urgent items, and everything else stays in the digest.
These tiny automations add up. One study of emergency physicians showed that batching non‑urgent pages saved an average of 45 minutes per shift – time that could be redirected to patient care or a quick stretch.
What to watch out for
Delegation isn’t a free‑pass to skip oversight. You remain ultimately responsible for the outcome, so keep these checks in place:
Confirm the delegate’s competence before handing over a task.
Document the hand‑off in the patient’s record, noting who performed the action and when.
Set up a quick “post‑task” debrief if the task involves clinical risk.
When you embed these safeguards, you’ll feel confident that you’re not just shifting work, you’re strengthening the whole team.
Ready to test the waters? Grab a sticky note, write down the three most time‑draining non‑clinical tasks you face this week, and assign each to a colleague or an automation rule. Schedule a 10‑minute review tomorrow to see how the hand‑off went.
Remember, the goal of time management for physicians isn’t to become a robot; it’s to reclaim the moments that let you focus on patients, on teaching, and on the little things that keep you sane.
Step 6: Establish Routine Review and Continuous Improvement
Now that you’ve set up blocks, delegated tasks, and automated the obvious, the next question is: how do you know it’s actually working? The answer is simple – you need a habit of regular review. Think of it like a daily vitals check, but for your schedule.
Schedule a 10‑minute “time audit” at the end of each shift
Grab your phone or a sticky note and spend the last ten minutes of your day jotting down three things:
What went exactly as planned?
Which block got invaded and why?
One tweak you can make for tomorrow.
It’s not a deep dive; it’s a quick pulse. Over a week you’ll start seeing patterns – maybe that 2 pm batch‑paging slot always collides with a clinic hand‑off, or the morning chart‑review block consistently runs over because you’re waiting on labs.
Does that feel like extra work? Nope. It’s the same time you’d otherwise waste wondering why you felt rushed.
Turn observations into actionable tweaks
Pick one tiny adjustment per week. If your “no‑page” window is constantly broken by urgent lab alerts, shift the window 15 minutes later or add a quick “urgent‑only” filter in your pager system. If you notice you’re spending ten minutes scrolling through a chat app during a protected block, mute the group for that hour.
Remember, the goal isn’t perfection; it’s progress. Small, iterative changes add up faster than a massive overhaul that never sticks.
Weekly “reflection sprint”
Set aside a dedicated 20‑minute slot on Friday or Sunday – call it your “review sprint.” Pull your daily notes, tally up how many blocks stayed intact versus how many were breached, and give yourself a quick rating from 1‑5.
Use that rating to decide whether you need a bigger change. A 3 or below? Maybe it’s time to re‑evaluate the block length or add a buffer for unexpected calls. A 4‑5? Celebrate that win and lock the pattern in for the next cycle.
And if you need a little external perspective, the White Coat Investor outlines a similar weekly review loop for doctors looking to tighten their time management time‑management strategies for doctors .
Monthly KPI snapshot
While daily notes keep you honest, a monthly snapshot helps you see the bigger picture. Choose two or three key performance indicators (KPIs) that matter to you – for example:
Average patient‑to‑chart time
Number of non‑clinical interruptions per shift
Hours of protected personal time logged
Plot them in a simple line chart or even a spreadsheet. If you notice a steady climb in interruptions, that’s a red flag worth investigating.
Sharing the KPI sheet with a trusted colleague or a wellness coach can add accountability without feeling like a performance review.
Iterate, don’t overhaul
Continuous improvement is a loop, not a ladder. After each monthly review, pick one or two experiments for the next month. Maybe you’ll try a themed‑day approach for Tuesdays, or you’ll test a new EMR template that cuts documentation time by five minutes.
Give each experiment at least two weeks before judging its impact – otherwise you risk tossing out a potentially valuable tweak too soon.
Make review a team habit
Time management isn’t a solo sport. Invite your medical assistant or practice manager to the Friday sprint. Ask them to share what’s working on their side of the workflow. You might discover that a simple hand‑off checklist you created last month saved everyone ten minutes, but nobody mentioned it because it felt “obvious.”
When the whole team sees that the review process leads to tangible improvements, they’ll be more inclined to stick to the new routines.
Quick checklist to lock in the habit
Set a daily 10‑minute end‑of‑shift audit.
Pick one micro‑adjustment each week.
Reserve a 20‑minute weekly reflection sprint.
Track 2–3 KPI metrics monthly.
Share findings with a colleague or coach.
By turning review into a routine, you turn “time management for physicians” from a one‑off project into a living system that grows with you. The next time you walk out of a shift feeling like you’ve finally nailed your schedule, you’ll know it wasn’t luck – it was consistent, data‑driven tweaking.
FAQ
How can I start a time audit without adding more work?
Grab a pocket‑size notebook or open a note on your phone before your shift begins. Every time you switch tasks, jot a quick timestamp and a one‑word label—“chart,” “page,” “break.” It only takes a few seconds, and at the end of the day you’ll have a rough map of where the minutes went. Does that sound doable? Most physicians say the audit becomes invisible after a couple of days.
What’s the best way to batch non‑urgent pages on a busy shift?
Set two‑minute windows—say 9:10‑9:12 am and 2:20‑2:22 pm—where you silence the pager for everything except true emergencies. During those windows, process all the queued messages in one go. You’ll notice the “noise” shrinking dramatically, and you’ll reclaim roughly 30‑45 minutes per day. Try it once and ask yourself, “Did I feel less interrupted?”
How do I protect deep‑work blocks when emergencies keep popping up?
Mark your calendar with a bold “Do Not Disturb – Patient Care Focus” slot and share the label with your team. Pair it with a “code‑blue only” filter on your phone so only life‑threatening alerts break through. When an interruption does slip in, note it and address it after the block. Over time you’ll see a pattern of “what really needs my attention now.”
Which simple tool can help me track time without being a distraction?
Many clinicians swear by the free version of Toggl Track. One tap starts the timer, another stops it, and the app auto‑generates a summary you can glance at during your 10‑minute end‑of‑shift review. No complex setup, no learning curve—just raw data you can act on. Give it a week and see if the numbers surprise you.
How often should I review my schedule to keep it effective?
Treat the review like a daily vitals check. Spend five minutes at the end of each shift noting which blocks held, which were breached, and one tweak for tomorrow. Then, once a week, do a 20‑minute “reflection sprint” to spot trends and adjust block lengths. Consistency beats a quarterly overhaul every time.
Can delegation really save me minutes, and how do I do it safely?
Absolutely—if you hand off tasks that land in Quadrant III or IV. Write a one‑page SOP for common hand‑offs like refill requests or routine lab notifications, and store it where your medical assistant can access it. After each shift, glance at a delegation log: did anything bounce back to you? If not, you’ve just saved several minutes without compromising patient safety.
What small habit can I add today to improve my overall time management for physicians?
Start each morning with a two‑minute “priority scan.” Open your calendar, locate your biggest Quadrant II block, and mentally commit to defending it. Then, write down the single most likely interruption and plan a quick response (e.g., “batch pages at 10 am”). That tiny pause creates a mental anchor and often frees up 10‑15 minutes by the day’s end.
Conclusion
We've walked through the whole Eisenhower Matrix journey, from auditing your day to protecting deep‑work blocks and delegating the noise. If any part felt like a “light‑bulb moment,” that's the point—time management for physicians isn’t a rigid formula, it’s a habit you tweak as you go.
So, what’s the next step? Grab that two‑minute priority scan you’ve been hearing about, pick one Quadrant III task to hand off tomorrow, and lock a 30‑minute protected slot on your calendar. When you see the minutes add up, you’ll notice a shift in energy, not just a longer to‑do list.
Remember, consistency beats perfection. A quick end‑of‑shift audit, a weekly reflection sprint, and a willingness to adjust will keep your schedule from spiralling back into chaos. You’ve already seen how a simple batch‑paging window saved 45 minutes for Dr. Patel—imagine the ripple effect when you apply the same principle to your own workflow.
Finally, if you’re curious about a deeper dive into burnout‑proofing your practice, our e7D‑Wellness self‑assessment can give you a personalized wellbeing profile and actionable next steps. Give it a try, and turn the chaos of the day into a rhythm you control.
You’ll start seeing more breathing room and less burnout every week.





Comments