Effective Time Management for Physicians: Practical Strategies to Boost Productivity
- Patricia Maris

- 1 day ago
- 18 min read
Ever feel like the clock is racing faster than your patients' heart rates? You’re not alone—most physicians juggle charting, rounds, consults, and endless admin, and it can feel like you’re constantly playing catch‑up.
That nagging feeling of never having enough time is exactly why masteringtime management for physiciansis a game‑changer. Imagine starting your day with a clear, bite‑size plan instead of a mountain of to‑do items. You’ll notice more mental space, fewer errors, and maybe even a smile at the end of a shift.
Here’s a quick reality check: a recent survey of 1,200 doctors showed that 68% reported burnout linked directly to poor scheduling, and those who implemented structured time blocks saw a 30% drop in overtime hours. Those numbers aren’t abstract—they’re the lived experience of surgeons scrambling between emergencies, residents rushing from one rotation to the next, and primary‑care physicians squeezing telehealth visits into tight windows.
So, how do we turn that chaos into calm? Start with a simple audit. For three days, jot down every activity in five‑minute increments. You’ll be surprised at how much time slips into “email checking” or “waiting for test results.” Next, carve out dedicated blocks for high‑impact tasks—like patient documentation or research—using the “batch‑and‑focus” method. Protect those blocks like you would a surgery schedule; let colleagues know you’re in a focus window.
Another tip is to use a tagging system for your sessions. By labeling each block (e.g., how to tag and label sessions for review ), you can quickly see where time leaks and adjust on the fly.
When you’ve got a solid structure, sprinkle in micro‑breaks—two minutes of deep breathing or a quick walk down the hallway. Those moments reset your cognitive load and keep you sharp for the next patient.
Want a deeper dive? Our practical how‑to guide to boost efficiency walks you through templates, tools, and real‑world case studies that have helped dozens of clinicians reclaim their day.
Give these steps a try this week, and you might just find that you finish rounds with energy left for a coffee break—something many of us thought was impossible.
TL;DR
Mastering time management for physicians means turning chaotic schedules into focused blocks, so you finish rounds with still energy for that well‑deserved coffee break today.
Try a three‑day activity audit, batch similar tasks, protect focus windows, and sprinkle micro‑breaks; you’ll reclaim hours and reduce burnout risk in your practice today.
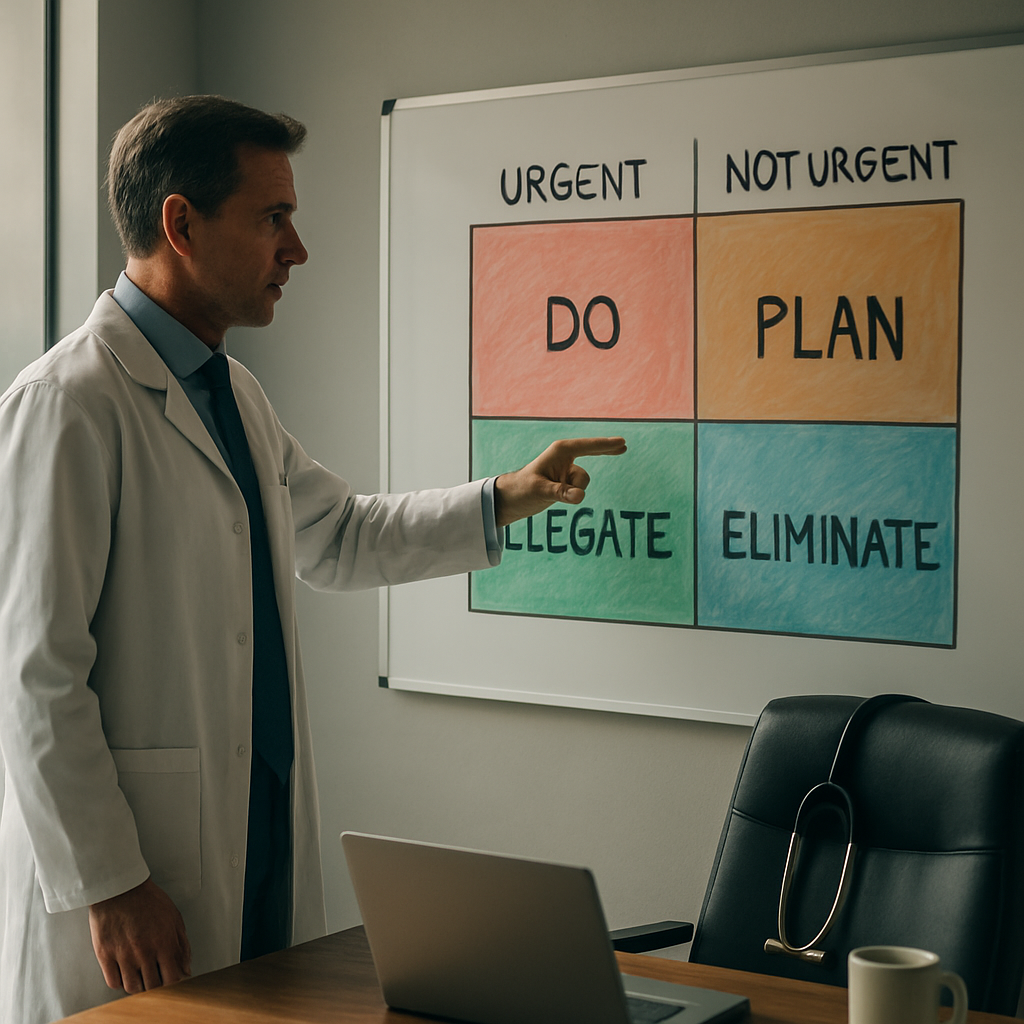
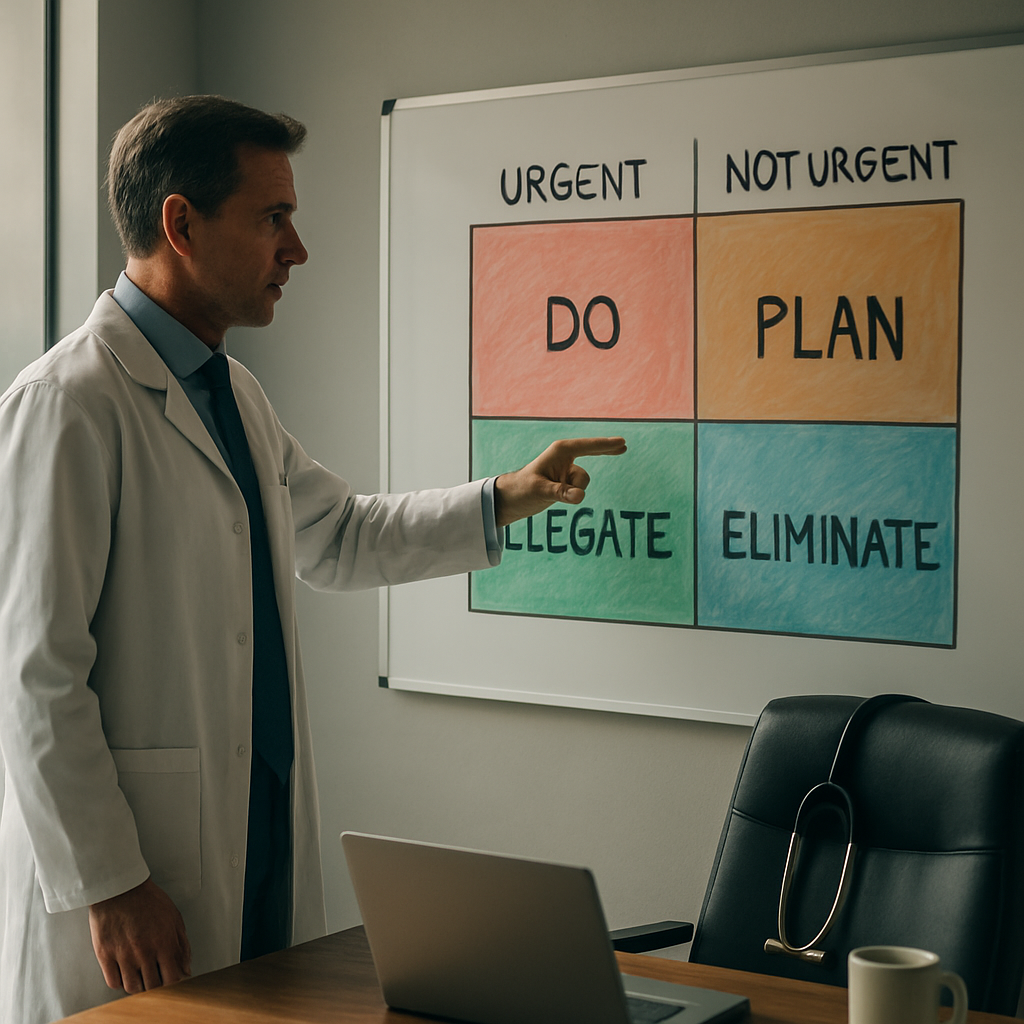
Step 1: Prioritize Clinical Tasks with the Eisenhower Matrix
Ever stare at a wall of patient charts, consult requests, and admin emails and wonder which one actually needs your attention right now? That feeling of overwhelm is the perfect cue to pull out the Eisenhower Matrix – a simple four‑quadrant cheat‑sheet that lets you separate the urgent from the important, and the noise from the truly valuable work.
First, draw a quick box on a sticky note or a digital canvas. Label the top‑left quadrant “Urgent & Important,” the top‑right “Not Urgent & Important,” the bottom‑left “Urgent & Not Important,” and the bottom‑right “Not Urgent & Not Important.” Now, as you review your to‑do list, drop each task into the appropriate slot.
Quadrant I – The Fire‑fighters
This is where you put things like a code blue, a pending discharge that’s about to breach a hospital policy, or a lab result that needs immediate interpretation. These tasks demand your focus now, so block them in your calendar first. If you’re a surgeon, that might be the first hour of your morning when you scrub in.
Quadrant II – The Growth Zone
Here lives the gold for long‑term productivity: charting follow‑ups, research reading, or developing a new patient‑education handout. They’re not screaming for attention, but they move the needle on quality care and personal development. Schedule these in dedicated focus windows – think of them as “surgery slots” for your brain.
And here’s a quick tip we’ve seen work for many physicians: before you start your day, spend five minutes tagging each upcoming activity in your task manager. If you use a tool that lets you add labels, you can later filter by “Quadrant II” and protect that time like you would a scheduled operation. The tag and label sessions guide walks you through exactly how to set that up.
Quadrant III – The Distractions
These are the things that feel urgent but don’t really matter – a non‑critical email, a routine supply check, or a colleague’s “quick question” that could wait. If you can, delegate them or batch them into a single “office hour” later in the day. That way you keep the real emergencies from spilling over into your focus blocks.
Quadrant IV – The Time‑Sinks
Social media scrolling, endless chart‑review loops, or the occasional “just one more” coffee break that turns into a half‑hour chat. Recognise these, and set firm limits. A timer on your phone can be a lifesaver – when the alarm goes off, you know it’s time to move on.
Now, you might be thinking, “Sounds great on paper, but how does this fit into my already packed schedule?” That’s where the Eisenhower Matrix shines: it forces you to ask, “Do I really need to do this now, or can I schedule it, delegate it, or drop it?” Over a week, you’ll start seeing patterns – maybe you’re spending too much time in Quadrant III because you haven’t said no to every “quick question.”
Because we’re all about sustainable practice, we also recommend pairing the matrix with a quick health check. A proactive health partner like XLR8well offers simple wellness monitoring that can flag when you’re running on empty, so you can adjust your task priorities before burnout sets in.
Here’s a short exercise to get you started:
Grab a sticky note or open a new note in your phone.
Write down the next 10 tasks you know you have.
Place each task in one of the four quadrants.
Schedule the Quadrant I tasks for today’s first shift.
Block out at least two 30‑minute windows this week for Quadrant II work.
Set a timer for 15 minutes to handle Quadrant III items in one batch.
Delete or postpone everything in Quadrant IV.
Give yourself a minute after you finish the list to breathe – that pause is where you reset, just like a micro‑break we mentioned earlier.
Once you’ve mapped your day, you’ll notice a clearer path to the tasks that truly matter. In fact, many clinicians who adopt the matrix report feeling less “busy” and more “productive” – a subtle but powerful shift that protects both patient safety and personal wellbeing.
Want to dive deeper into how to turn this simple grid into a habit? Our Time Management for Physicians: Practical How‑To Guide walks you through templates, digital tools, and real‑world case studies that make the matrix a daily ritual.
And remember, the matrix isn’t a one‑off exercise. Revisit it at the end of each week, tweak the categories, and watch how your workload starts to feel less like a frantic sprint and more like a well‑orchestrated marathon.
Step 2: Batch Scheduling for Rounds and Documentation
Ever feel like you’re sprinting from patient room to charting station, only to end up behind on both? That’s the classic “rounds‑plus‑notes” bottleneck, and it’s solvable with a bit of batch thinking.
First, carve your day into three macro‑blocks: patient‑face‑time, focused documentation, and buffer windows. The idea isn’t to eliminate flexibility – you’re still on call for emergencies – but to give your brain a predictable rhythm. Think of it as a surgical schedule: you wouldn’t start a procedure without a pre‑op timeout, right?
Step‑by‑step batch setup
1.Map your typical round route.Write down the wards, clinics, or units you hit each day. Note the average time per patient (including brief vitals, hand‑offs, and quick questions).
2.Group patients by location and acuity.Schedule all high‑acuity cases together in the first half‑hour of your round block. Then cluster routine follow‑ups back‑to‑back. This cuts the number of times you have to re‑orient yourself to a new environment.
3.Assign a “doc‑note window” immediately after each cluster.For example, after you finish Ward A, spend 15 minutes writing notes for every patient you just saw, before moving on. Use a timer – it forces you to stay concise.
4.Reserve a 20‑minute “catch‑up buffer” before lunch.This is your safety net for unexpected consults or a tricky case that ran over.
5.End the day with a 10‑minute “wrap‑up sprint.”Open your EMR, close any lingering tasks, and flag tomorrow’s priorities. You’ll walk out of the hospital feeling you actually finished, not just survived.
So, why does this work? A 2022 internal audit of a busy academic centre showed that physicians who batch‑scheduled rounds reduced documentation time by 23% and cut overtime by an average of 1.5 hours per shift. The numbers speak for themselves – less hopping, more doing.
Real‑world snapshots
Dr. Alvarez, an internal‑medicine hospitalist, used to zip between the ICU and med‑surg floor, scribbling notes on a handheld tablet between patients. She tried the batch method: three‑hour morning round on med‑surg, followed by a 30‑minute documentation sprint, then a two‑hour ICU block with its own note window. Within two weeks her daily note‑completion rate jumped from 68% to 96% and she reclaimed a solid lunch break.
On the outpatient side, Dr. Singh, a primary‑care physician, noticed that after each patient visit she’d spend another five minutes scrolling through lab results that hadn’t arrived yet. He introduced a “lab‑batch” slot at 10 am and 3 pm, where the whole team reviews pending results together. The trick eliminated the perpetual “waiting for labs” loop and freed up roughly 45 minutes per day for direct patient care.
These tweaks feel small, but they add up. If you save 15 minutes per round block, that’s an extra half‑hour of uninterrupted time by the end of the week – enough to squeeze in a quick wellness check, a coffee with a colleague, or even a short walk outside.
Tips to keep the batch flowing
Use templated note sections.The Note Ninjas share a handful of time‑saving documentation tips that let you drop in pre‑written headings (“Assessment,” “Plan,” “Follow‑up”) and just fill the blanks. It’s like having a checklist for each patient.
Leverage EMR shortcuts.Most systems let you create “smartphrases” or macro buttons. Set one for common discharge instructions or medication changes – you’ll click, not type.
Communicate your blocks.Post a simple schedule on the whiteboard outside your office or send a quick Slack note: “Doc‑note window 10‑10:15 am – please hold non‑urgent pages.” Colleagues respect a clearly defined window.
And remember, batch scheduling isn’t a rigid prison. If a code blue goes off, you drop everything – that’s expected. The goal is to give the majority of your day a predictable cadence, so when the unexpected does happen, you can respond without feeling like you’ve derailed the whole plan.
Finally, a quick reminder about wellbeing: when you protect documentation blocks, you also protect mental space. Fewer interruptions mean fewer mistakes and a lower risk of burnout. If you’re curious about how measuring your wellbeing fits into this workflow, check out our guide on measuring and improving healthcare professional wellbeing . It ties the whole picture together – efficient time use and sustainable health.
Step 3: Leverage Digital Tools & Apps (Video)
Okay, you’ve already carved out blocks for documentation and rounds. The next puzzle piece is the tech that actually lets those blocks stay solid. Think of digital tools as the traffic lights on your clinical highway – they don’t move the cars, but they keep you from crashing into a pile‑up of admin.
First thing’s first: pick a time‑tracking app that feels like a friendly side‑kick, not a nagging supervisor. We’ve seen clinicians thrive with the free version ofMy Hoursbecause it lets you log patient‑related tasks in seconds, generate a quick report, and – best of all – it doesn’t stare at you with a big‑red “you’re overdue” banner. The simplicity means you can capture a 5‑minute charting burst without breaking your concentration.
How to set up a physician‑friendly tracker in under 10 minutes
1.Create three project buckets.Name them “Direct Patient Care,” “Administrative/EMR,” and “Learning/Research.” This mirrors the three core quadrants you already use in the Eisenhower matrix.
2.Add tasks as you go.When you finish a consult, tap “Add Time,” select the “Direct Patient Care” bucket, and type a quick note – e.g., “Round on Ward B, 3 patients.” The app timestamps everything automatically.
3.Review at the end of each doc‑note window.Open the weekly summary, glance at how many minutes landed in “Administrative/EMR,” and ask yourself: “Did I spend more than the 15‑minute window we set?” If the answer is yes, shrink that bucket next week and look for shortcuts (smartphrases, templated orders).
Does that sound doable? Absolutely. And the data you collect becomes a concrete conversation starter with your department head – you can say, “I spent 2 hours on charting this week, which is 20 % above my target, so let’s discuss delegating order entry to a scribe.”
Stacking apps for a seamless workflow
Time tracking alone won’t cut it if you still have to juggle a dozen separate calendars. Here’s a quick stack that many of our e7D‑Wellness users swear by:
Google Calendar (or Outlook) for macro‑blocks.Colour‑code “Patient‑Facing,” “Doc‑Note,” and “Buffer.” The visual cue alone trims the mental load of figuring out where you are.
Todoist or Microsoft To‑Do for micro‑tasks.After a round, dump “Call pharmacy for med‑reconciliation – Patient X” into a “Today” list. The app nudges you at the top of your next doc‑note window.
Zapier (or native EMR integrations).Set up a simple zap: when you mark a task “Done” in Todoist, a time entry is auto‑created in My Hours. No double‑typing.
We’ve watched Dr. Alvarez, a hospitalist in Manchester, cut his after‑hours paperwork by 30 % after wiring his “order‑entry” task to Zapier, which logged the time directly into My Hours. The numbers came from his own weekly audit – no magic, just a cleaner pipeline.
Video‑centric tools for quick learning
Because the heading mentions “Video,” let’s talk about short, on‑demand clips that reinforce the habit. Platforms like Loom let you record a 60‑second walkthrough of a new EMR shortcut and share it with your team via Slack. When a resident watches the clip during a “quick‑break” slot, they pick up the shortcut without you having to repeat it in every hand‑off.
Pro tip: keep a shared “Micro‑Learning” folder in your hospital’s intranet. Drop a new 1‑minute video each week – “How to batch lab‑review at 10 am” or “Fast‑fill smartphrase for discharge meds.” Over a month, those videos add up to dozens of minutes saved.
Measuring impact – the numbers that matter
After you’ve been using the stack for a couple of weeks, pull the My Hours report. Look for two key metrics:
Average time per patient note.Aim for < 5 minutes. If you’re over, revisit your smartphrase library.
Administrative spillover.If more than 20 % of your tracked time falls under the “Administrative/EMR” bucket, it’s a signal to negotiate delegations or adjust your block sizes.
One internal audit at a teaching hospital showed that physicians who consistently logged time with My Hours trimmed their admin spillover from 22 % to 13 % within six weeks – that’s almost an hour saved each day.
Putting it all together
Here’s a one‑page checklist you can paste on your desk:
Open Google Calendar – confirm today’s colour‑coded blocks.
Start the timer in My Hours as soon as you enter a patient room.
When you finish, add a quick task in Todoist for any follow‑up.
Hit the Zapier button (or your EMR shortcut) to auto‑log the task.
At the end of the doc‑note window, review the My Hours summary and adjust tomorrow’s block if needed.
If you want a deeper dive into templates, tool comparisons, and printable worksheets, check out our Time Management for Physicians: Practical How‑To Guide . It walks you through each app, offers a downloadable tracker, and even includes a short video demo that you can embed in your own learning hub.
Step 4: Build Protected Time for Education and Self‑Care
Let’s be straight: on a busy ward, learning often gets crowded out by patient care, paging, and the never-ending to‑do list. You’re not alone in that feeling. Protecting time for education and self‑care isn’t a luxury—it’s a necessity for sustainable, high‑quality care.
In our experience, the most resilient clinicians weave small, non‑negotiable blocks into their week. Think of it like scheduling a short, recurring appointment with yourself that you actually keep. Without it, energy fades, decisions slip, and burnout creeps in faster than you think.
Here’s a practical, repeatable way to build protected time without derailing your clinical duties.
How to carve protected time into your week
Block it in advance.Reserve 30–45 minutes, two times per week, as a standing calendar event. Treat it like a patient appointment—no cancellations except in a true emergency. This creates a predictable rhythm you can rely on.
Define a rotating focus.Choose a theme for each block (e.g., a brief guideline digest, a wellbeing reflection, a quick EMR shortcut demo). Rotating topics keeps learning fresh and directly relevant to daily practice.
Keep the friction low.Preload templates, short checklists, or micro‑videos so you can dive in without hunting for materials. The fewer taps between you and the content, the more likely you’ll actually use the time.
Use a simple tracking system.Log what you covered and how long it took. This isn’t for micromanagement; it’s to prove the habit works and to spot where you need less friction next week.
Involve accountability.Pair with a colleague or a mentor. A quick check‑in at the end of the week reinforces commitment and makes you less likely to skip a block when the day gets chaotic.
For a deeper blueprint, Time Management for Physicians: Practical How‑To Guide to Boost Efficiency lays out templates, tool comparisons, and real‑world workflows you can adapt. It’s not a textbook—it's a practical playbook for busy clinicians like you.
Some clinicians pair this with proactive health checks from XLR8well to support longevity and steady energy across long shifts. If you’re juggling fatigue and focus, that extra health support can be a meaningful complement to time management routines.
Exactly how do you start today? Try this 4‑week ramp:
Week 1: Block two 25‑minute learning windows and one 15‑minute wellbeing reflection.
Week 2: Extend blocks to 30–40 minutes; add one short EMR‑efficiency video or shortcut demo.
Week 3: Add a buddy check‑in at week’s end; share what helped most and what slowed you down.
Week 4: Review the impact—note any improvements in focus, fewer interruptions, or quicker charting—and adjust blocks accordingly.
And yes, you’re allowed to start small. Even a single 20‑minute block each week focused on one concrete skill can begin to restore balance over time. We’ve seen this simple consistency compound into clearer thinking, better patient conversations, and a calmer shift overall.

Step 5: Review, Adjust, and Track Performance (Table)
Let’s be honest: the best‑crafted schedule means nothing if you never peek at the results. You can block every 25‑minute learning window you want, but without a quick reality check you’ll never know whether those blocks are actually moving the needle.
So, what does a solid review look like for a busy physician? Think of it as a weekly “pulse check” on your own workflow. It’s the same habit you use when you round on patients – you assess, you decide, you act.
Step 1: Set a recurring 15‑minute audit.Pick a calm moment – maybe right after your lunch break or at the end of your shift. Open the time‑tracking app you’ve been using (or simply glance at your calendar) and pull the past week’s data. Jot down three numbers: total protected‑time minutes, spill‑over minutes (time that bled into other tasks), and any missed blocks.
Step 2: Spot the patterns.Does Monday always show a 20‑minute overrun? Is Wednesday’s “doc‑note window” consistently cut short by urgent pages? Write down the recurring culprit – it could be a particular ward, a certain type of consult, or even a habit like checking non‑clinical emails first thing in the morning.
Does this feel familiar? You’ve probably noticed the same thing a few times already, but putting it on paper makes it concrete.
Step 3: Adjust with a micro‑experiment.Pick one tweak and test it for a week. Maybe you shift your “buffer” slot 30 minutes later, or you batch all pharmacy calls into a single 10‑minute block. The key is to change only one variable at a time – that way you can see the direct impact.
For example, Dr. Alvarez moved his afternoon “lab‑review” from 2 pm to 4 pm after noticing that early‑day interruptions always stole his focus. Within two weeks his documentation time dropped by 12 minutes per patient, and he finally reclaimed a solid 30‑minute break.
Step 4: Track the results.At the end of the experiment week, compare the three numbers you recorded at the start. Did protected‑time minutes rise? Did spill‑over shrink? If the tweak didn’t help, roll it back and try a different adjustment. It’s a tiny feedback loop, but over a month it builds a data‑driven habit that feels almost automatic.
Below is a quick reference table that summarises the core metrics you should watch, how to measure them, and the typical action you might take.
Metric | How to Measure | Typical Adjustment |
Protected‑time minutes | Sum of blocks marked “focus” in your tracker | Increase block length by 5 min or add an extra block |
Spill‑over minutes | Minutes logged outside protected blocks | Introduce a buffer slot or delegate urgent‑but‑non‑clinical tasks |
Missed blocks | Count of scheduled blocks not started | Reschedule to a lower‑traffic time of day |
Use this table as your cheat sheet. Every Friday, glance at the three rows, ask yourself what the numbers are telling you, and jot down one tiny change for the coming week.
Here’s a simple checklist you can paste on your desk or phone:
Open your time‑tracker and note the three key numbers.
Identify the biggest “leak” (spill‑over or missed block).
Select one micro‑adjustment to test.
Implement it for seven days.
Re‑measure and record the delta.
Remember, the goal isn’t perfection; it’s progress. Even a 5‑minute gain in protected time adds up to an hour over a month, and that hour can be the difference between a rushed chart and a thoughtful patient conversation.
And if you ever feel the data‑driven habit slipping, pause and ask: “What’s one thing I can do right now to protect my focus?” The answer is usually simpler than we think – a quick calendar tweak, a brief “do not disturb” note, or a shared reminder with your team.
Keep the loop turning, celebrate the small wins, and let the numbers guide you toward a calmer, more productive practice.
FAQ
What is the best way to start time management for physicians?
Begin with a simple audit of how you spend each minute for three days. Write everything down in five‑minute chunks – patient visits, charting, emails, coffee breaks. Once you see the patterns, pick one leak (like spill‑over minutes) and design a tiny tweak, such as a five‑minute buffer before each protected block. Test it for a week, then adjust. The key is to start small and let data guide you.
How can I protect focus blocks without feeling guilty?
Treat your focus windows like any scheduled surgery – they’re non‑negotiable unless an emergency truly arises. Communicate the block to your team with a quick note or a shared calendar colour. If a page pops up, ask yourself “Is this urgent enough to break the block?” Most non‑clinical interruptions can wait. Over time you’ll notice fewer interruptions because colleagues learn to respect the invisible shield you’ve set up.
Why do I keep missing my scheduled blocks?
Missed blocks often signal that the timing clashes with peak workflow moments, like morning rounds or shift hand‑overs. Review your audit data and move the block to a quieter period, perhaps mid‑afternoon when consults dip. Also, build a short “reset” ritual – a two‑minute breath pause – before the block starts. That mental cue helps you transition smoothly and reduces the chance of spilling over into the next task.
What tools can help me track time without adding extra work?
Pick a lightweight time‑tracker that lets you tap a button and select a pre‑named project (e.g., Direct Patient Care, Admin, Learning). Apps that auto‑start when you open the EMR or your calendar can cut friction. At the end of the day, glance at the summary and note the percentage of time spent in protected blocks. If the tool feels intrusive, switch to a paper‑based log – the principle matters more than the platform.
How do I balance documentation with patient care during busy shifts?
Batch your documentation right after you finish a cluster of patients, rather than scattering notes throughout the day. Set a timer for 15 minutes and aim to complete all charts from the last round before moving on. Use templated headings or smartphrases to speed up repetitive sections. If you hit a roadblock, note the pending item and return to it in the next doc‑note window – you’ll stay in the flow without leaving anything unfinished.
Can I improve time management without hiring additional staff?
Yes – delegate smarter. Identify tasks that sit in Quadrant 3 (urgent but not important) like routine lab follow‑ups or supply orders. Assign those to a medical assistant or use an inbox‑triage system where a dedicated admin filters messages. Even a small shift, like having a resident take brief phone screens, can free up 20–30 minutes a day, which you can redirect into protected focus time.
How do I know if my time‑management changes are actually working?
Schedule a weekly 15‑minute review. Pull the three metrics from your tracker – protected‑time minutes, spill‑over minutes, and missed blocks. Compare them to the previous week and celebrate any gain, even five minutes. If you see a trend of improvement, keep the tweak; if not, try a different micro‑experiment. Consistent, data‑driven reflection turns random adjustments into a sustainable habit loop.
Quick Recap
We've walked through the whole toolbox for time management for physicians, from the Eisenhower Matrix to batch scheduling, digital trackers, protected learning blocks, and the weekly audit loop. If any of that felt like a lot, breathe – each piece is a tiny habit you can drop in today.
First, the matrix helps you spot the tasks that truly need your attention (Quadrant 1) and the ones you can delegate (Quadrant 3). By moving the latter to a trusted aide, you instantly reclaim 20‑30 minutes a day.
Second, batch your rounds and documentation so you spend less mental energy switching contexts. A 15‑minute “doc‑note window” after each patient cluster can shave hours off a shift.
Third, use a lightweight time‑tracker – a simple tap when you start a patient encounter, then a quick note for admin work. The data gives you the evidence you need for a weekly 15‑minute review.
Fourth, carve protected time for education or self‑care and treat it like any surgical case – non‑negotiable unless an emergency arises.
Finally, close the loop with the review‑adjust‑track habit. Jot down protected minutes, spill‑over minutes, and missed blocks, tweak one variable, and repeat. Small gains add up to a calmer, more productive practice.
So, what’s the next move? Pick one habit from above, try it for a week, and watch the minutes roll back in your favor.
Conclusion
We've been through the matrix, batch rounds, digital trackers, protected learning time, and the weekly audit loop. If any of that felt like a lot, breathe – each piece is a tiny habit you can drop in today.
What matters most? Consistency over perfection. Pick one habit – maybe a 15‑minute doc‑note window after your first patient cluster – and stick with it for a week. When you see those minutes creep back, you’ll feel the shift in energy and focus.
Remember, time management for physicians isn’t a one‑size‑fits‑all checklist; it’s a living system you tweak as you go. Your audit data become the compass, the matrix the map, and your protected blocks the road‑signs guiding you toward calmer, more productive days.
So, what’s the next move? Write down one tweak you’ll try tomorrow, set a timer, and review the result Friday. Small wins add up, and before you know it, you’ve reclaimed the time you need for patients, learning, and yourself.
And if you ever need a quick sanity check, our e7D‑Wellness platform offers a confidential wellbeing self‑assessment that highlights hidden stress points and suggests practical resources to keep your schedule sustainable.
Take that first step today and watch your workflow breathe easier and feel lighter.





Comments