ACGME Wellness Requirements 2026: Complete Guide for Residency Programs
- Patricia Maris

- 1 day ago
- 16 min read

Ever feel like the clock is chasing you, not the other way around? You’re not alone. Every clinician who’s walked the wards at night or paced the waiting room knows the hum of exhaustion. It’s not just a personal struggle—it’s a signal that the system is asking for help. ACGME has put wellness on the radar, and that’s where we come in.
The ACGME wellness mandate isn’t a trendy checkbox; it’s a framework that forces programs to track sleep, burnout, and workload. Think of it as a safety net for a high‑stakes sport—one that catches you before you fall. For many residency programs, it’s a daily balancing act between clinical duties and personal well‑being.
Picture Dr. Maya, a surgical resident who’s logged 90‑hour shifts for two weeks straight. She’s still nursing a sore throat, juggling exams, and trying to find time to stretch. When she finally fills out the wellness questionnaire, she discovers her score is below the program’s threshold. That’s the moment the ACGME steps in—prompting an intervention that could shift her trajectory.
What’s the secret sauce? It’s a data‑driven approach that turns subjective feelings into measurable metrics. Programs start by mapping hours, tracking mood, and setting benchmarks for rest. The data then fuels conversations with residents, making wellness an actionable priority instead of a vague aspiration.
If you’re wondering where to begin, the first tool that can save you hours is a simple, ACGME Wellness Requirements Checklist for Programs . It lays out every requirement side by side, so you can tick off compliance with confidence. Think of it as your personal wellness compass for 2026 and beyond.
That checklist isn’t just paperwork—it’s a roadmap. By aligning your duty hours, sleep cycles, and debrief sessions, you create a cycle of feedback that keeps wellness in the forefront. And because it’s so straightforward, even the busiest clinic can incorporate it without adding another layer of admin.
But checklists are just the tip of the iceberg. To really hit the mark, you need systems that help you label and tag each session—whether it’s a patient encounter or a debrief meeting. How to Tag and Label Sessions for Review: A Practical Step‑by‑Step Guide can cut through the paperwork maze and make compliance feel like a natural part of your workflow.
Take the next step by downloading the checklist and pairing it with a streamlined workflow system. If you’re looking for a concrete way to organize your patient notes and wellness data, this guide on session tagging is a game changer. Stay on top of your well‑being, and let the system do the heavy lifting while you focus on what matters most.
TL;DR
The ACGME wellness requirements mandate that residency programs track sleep, workload, and burnout, turning vague wellness talk into measurable checkpoints. With our checklist and session‑tagging guide, you can hit those metrics effortlessly, keeping clinicians and compliant—so the next time a resident logs a shift, their wellbeing is on your radar.
Understanding the 2026 ACGME Wellness Requirements
Let’s cut to the chase: in 2026, the ACGME wellness requirements stop being a vague mandate and start guiding real clinical practice. For clinicians and the residency programs that train them, that shift lands with heartbeats, it's not a box to check, it's a daily operating rhythm.
What changes, exactly? The core idea is simple: quantify sleep, workload, and burnout, then use that data to drive targeted interventions that actually improve daily life on the ward, in the ICU, or in clinic. You’re not aiming for perfection; you’re aiming for predictability so residents sleep more, show up rested, and feel supported.
For a practical starting point, download the ACGME Wellness Requirements Checklist for Programs . It aligns your duties with the metrics the board will review and helps you map gaps quickly.
What gets measured in 2026
Duty hours and scheduled rest periods
Sleep quality and duration across shifts
Burnout indicators, mood trends, and perceived support
Debrief quality, peer interactions, and supervision adequacy
Interventions implemented, with tracking of outcomes over time
Team workload balance and coverage gaps that push clinicians to overwork
Patient-safety alerts linked to wellness data (where applicable)
Compliance milestones and program-level dashboards for oversight
Notice how this isn’t about micromanaging every minute of a shift. It’s about turning subjective wellbeing into objective data you can discuss with residents and leaders, so you can spot patterns and intervene early.
In our experience, the combination of a simple checklist and a lightweight workflow—where you label sessions with context and pull quarterly summaries—makes compliance feel practical, not punitive. It builds a shared language around rest, workload, and support, which matters more than any single metric.
Here’s how to start turning data into real change: collect hours, sleep data, and mood weekly; tag clinical encounters with contextual notes; and review trends in a monthly debrief that includes a short action plan for the next period.
Here's a quick explainer to see how teams turn data into action:
For practical coverage options, consider this resource: Group Health Insurance for Contractors: A Complete Guide to Coverage Options.
And for sleep support during night rotations, Yetibeds offers practical guidance: Yetibeds .
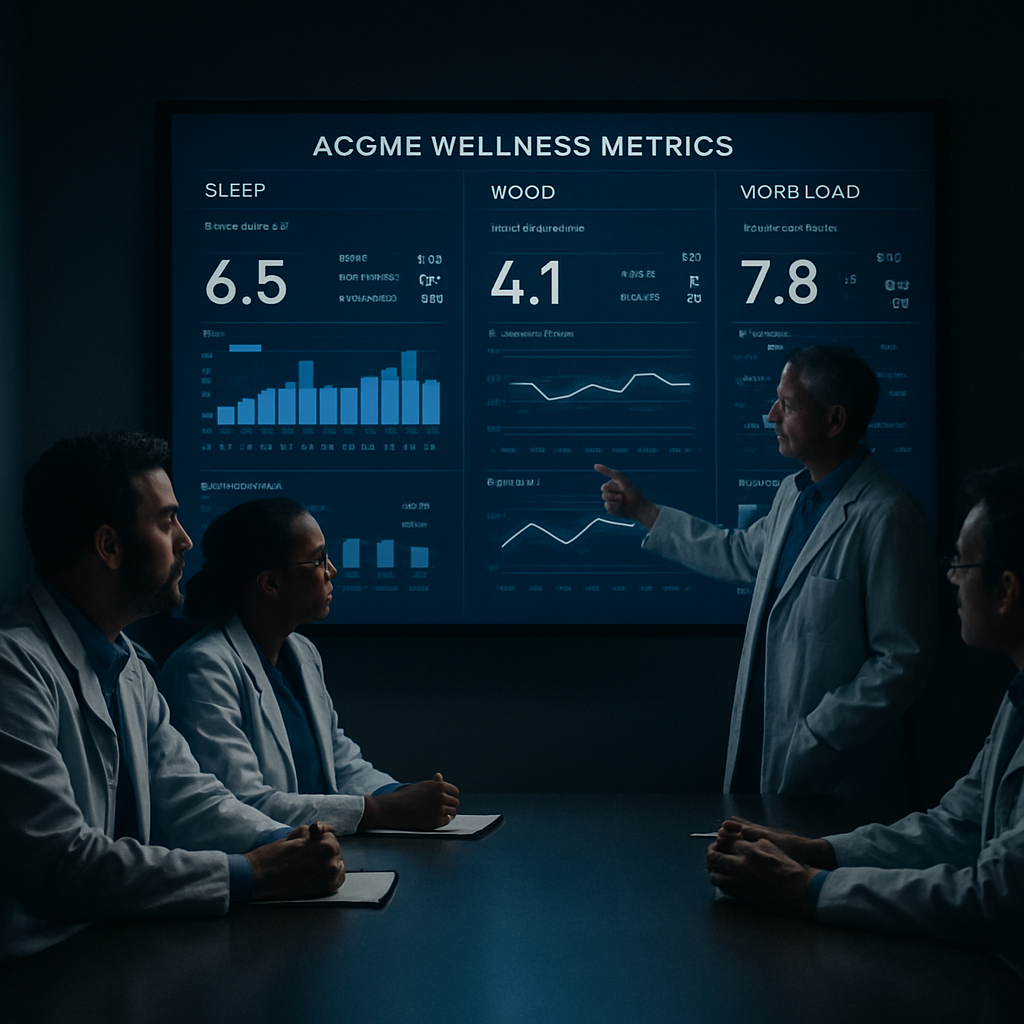
Imagine this on your program wall—a live dashboard tracking rest, workload, and burnout signals, with automated flags and owner accountability. The image below captures the concept in a cinematic, hospital‑focused moment.
With 2026 on the horizon, turning policy into practice is within reach for every residency program.
Key Wellness Domains and Mandatory Competencies
Let me be honest: if you're responsible for clinician wellness, you're juggling patient safety, staffing realities, and your own sanity. The 2026 ACGME wellness requirements aren't a checkbox; they're a practical map to safer care and sustainable careers.
Think of three core pillars as the backbone: Sleep and Rest, Workload and Scheduling, and Burnout Monitoring. When you get these aligned, fatigue signs turn into early alerts, and you keep the care pipeline flowing without burning people out.
Sleep and Rest: Protect the recovery window
You’re only as sharp as your last nap. Programs that codify protected rest windows, explicit post‑call recovery time, and routine mood checks tend to see fewer errors and sharper decision‑making on the floor.
Action helps here: schedule protected blocks for rest, approve after‑call unwind time, and offer flexible napping strategies for night shifts. If you’re curious about how to structure this, the practical steps below translate directly into daily practice you can start next week.
Catalog every shift type and its duration, so you know where rest windows fit and where you need coverage buffers.
Block protected rest periods—aim for consistent sleep opportunities, even if it means micro-naps during long night floats.
Establish a 5‑minute post‑shift debrief to reset before residents leave the unit.
For a practical, program-ready starting point, see the ACGME Wellness Requirements Checklist for Programs .
Workload and Scheduling: Make work predictable
Predictability reduces cognitive load and fatigue. Map duty hours with clear maximums, design surge coverage protocols, and create a transparent system so residents know what to expect and when to ask for help.
Think in terms of flow rather than chaos: distribute high‑acuity periods evenly, embed mentorship touchpoints during busy weeks, and build in built-in buffers for handoffs and documentation. When schedules feel fair, morale follows and so does steadier patient care.
Publish a weekly schedule two weeks in advance and lock in protected time for teaching, debriefs, and rest.
Include explicit buffers for admin tasks, handoffs, and unpredictable patient surges.
Use a simple tagging system to flag high‑acuity periods for proactive mentorship and resource referrals.
Burnout Monitoring and Early Warning Signs
Yearly surveys aren’t enough. You need lightweight, confidential screens embedded in the daily workflow, plus clear escalation and support paths. Combine mood tracking with workload data so leadership sees trends, not just isolated data points.
Actionable steps: implement a quick burnout screen residents can complete in under two minutes, schedule mentor conversations within 48–72 hours of a flagged result, and translate the data into a leadership dashboard that highlights at‑risk teams before burnout becomes a crisis.
Adopt a compact burnout screen that’s confidential and easy to complete.
Pair each high‑risk signal with a prompt mentor discussion and resource referral.
Review aggregated mood, sleep, and workload data monthly to catch patterns early.
In our experience, platforms like e7D‑Wellness support these objectives by providing confidential self‑assessments and data‑driven insights that surface early risk signals and guide practical action.
Need context from the official guidance? The 2026 ACGME standards for internal medicine outline these pillars and the required workflow integrations—worth a quick read if you’re building program policy ACGME 2026 Internal Medicine Requirements.
So, what should you do next? Map your shifts, protect rest windows, pilot a 5‑minute debrief, and implement a lightweight burnout screen. Start small, track what changes, and scale what works—one practical step at a time.
And if you’re ready to turn this into daily practice, remember: consistency beats intensity when it comes to clinician wellness and patient safety in 2026 and beyond.
Assessment Tools and Data Collection Methods
Let’s get practical. Assessment tools and data collection aren’t about busywork—they’re the map to safer, calmer care.
The goal is to turn subjective feelings into trackable signals you can act on, without drowning in forms.
We lean on lightweight, confidential self-assessments, mood and sleep logs, and workload metrics that teams can review regularly.
Key components include a quick burnout screen (under two minutes), a simple mood inventory, shift hours, and debrief outcomes.
Data collection should be embedded in daily routines: post-shift huddle, mentoring conversations, and calendar prompts.
A dashboard that surfaces trends before they spike is the backbone of timely support.
That image isn’t just for show. Think of it as a practical guide you can reference in real time during a shift change or a mentorship huddle.
For context on official guidance, you can consult the 2026 ACGME wellness requirements and related resources. ACGME Public Health General Preventive Medicine requirements (PDF).
If you’re looking for a practical starter, check out the residency-focused overview. ACGME Wellness Requirements for Residency Programs give you a grounded, policy-to-practice path you can map to your program calendar.
Here's a quick explainer video to ground these ideas.
Think of the dashboard as a living map—it's not a report card, it's a guide to where to act next.
Does this really work? In clinical teams, small, repeatable data hooks beat massive, once-a-year surveys.
And it scales: one confident clinic, then another, then the whole program.
Keep it lightweight: two minutes to answer mood, one to log hours, and a 5‑minute debrief.
In our experience, the right data workflow saves time and protects patient safety.
Remember, the best tools disappear into the workflow when they’re truly useful.
If you want more templates, we’ve got practical checklists and dashboards that fit busy residency programs.
One more tip: pilot the data collection with a single cohort first, then capture feedback and refine.
The data also informs leadership dashboards that flag at‑risk teams before a crisis.
So yes, this is doable—one step at a time, with the right pace and the right supports.
Benchmarking Across Programs: A Comparison Table
Let’s get practical. Benchmarking across residency programs isn’t about chasing shiny numbers. It’s about turning subjective vibes, like sleep debt and burnout signals, into apples-to-apples insights you can actually act on.
Think of benchmarking as a map you can trust. Pick a handful of core areas, collect the same signals from each cohort, and compare them over time. The goal isn’t to rank programs; it’s to spot patterns and intervene before small problems snowball.
In our experience at e7D-Wellness, a lightweight data load works best: mood checks, hours logged, and a brief after-action debrief. When you keep the data simple, teams actually use it and leaders can spot trends without drowning in dashboards.
For a practical starting point, the ACGME Wellness Requirements Checklist for Programs provides a straightforward, program-ready framework you can map to your calendar. ACGME Wellness Requirements Checklist for Programs .
Benchmark Area | Option / Tool | Key Metrics | Notes |
Sleep & Rest | Protected rest windows + post-shift unwind | Average sleep hours per 24h; rest window adherence | Look for consistency across rotations; aim for steady recovery |
Workload & Scheduling | Structured duty-hour blocks + debriefs | Shift length, handoff count, admin time | Plan for predictable cycles; include buffers for surges |
Burnout Monitoring | Confidential quick burnout screen | Two-minute mood/burnout score; time to mentor response | Flag early signals; tie to mentorship resources |
Leadership Oversight | Leadership dashboard with at-a-glance risk indicators | At-risk cohorts, trend lines, response timeliness | Review monthly; ensure actions translate to scheduling decisions |
Interventions & Action | Targeted mentorship, rest facilitation | Intervention response time, actions taken | Close the loop between data and support |
Data Privacy & Trust | Anonymous data collection, access control | Consent rate, data breach risk | Maintains trust and compliance across cohorts |
So, how do you actually use this table in real life? Start with one program cohort. Establish a baseline in the first 4 to 6 weeks, set clear 90-day targets, and review progress monthly. If a metric drifts—sleep drops or burnout risk climbs—trigger a targeted intervention, not a flood of new forms.
As you scale, replicate the same framework across additional tracks. The beauty is in the comparison: you’ll see where a rotation needs more mentorship, better handoffs, or a lighter call burden, and you can apply those learnings program-wide.
At our practice, we see the impact when wellness data informs scheduling and mentorship decisions. The data stays lightweight, privacy-respecting, and action-oriented. Start small, stay consistent, and let the map guide your next best steps. And if you want practical templates to accelerate adoption, we can tailor simple checklists and dashboards that fit busy residency programs.
Now, a quick reality check: 2026 wellness standards aren’t a one-off task. They’re a daily practice of turning signals into support. With this benchmarking table, you’ll have a clear, repeatable path to improve clinician well-being while safeguarding patient safety.
Implementation Strategies for Residency Program Directors
Let me level with you: turning wellness guidelines into daily hospital practice isn’t glamorous, but it’s non‑negotiable. You’re juggling patient safety, resident education, and workforce realities all at once. And yes, it can feel like spinning plates. So what should you do first?
Step 1: Establish baseline and governance
Draft a small wellness governance group that includes program leadership, chief residents, nursing representatives, and a patient‑safety liaison. Define exactly what you’ll measure: sleep opportunities (protected rest blocks), workload balance (duty‑hour predictability and admin time), and burnout signals (confidential mood checks). Agree on a simple data‑collection method—one dashboard, one weekly report—so you’re not chasing a dozen formats. Set 90‑day targets and a monthly cadence for review. In our experience, clarity here prevents paralysis and earns frontline trust.
Step 2: Map shifts and protect rest
Start with a thorough shift inventory: type, duration, variability, and peak load weeks. Block protected rest windows and after‑call unwind time; ensure coverage buffers are explicit in the schedule. Create a 5‑minute post‑shift debrief ritual to capture a quick learning and reset mood. Standardize handoffs to reduce cognitive load during transitions. When you present these changes, keep the language practical: what changes, who approves, when does it start?
Shift types and duration mapped
Protected rest blocks in every schedule
Clear post‑call unwind and debrief requirements
Step 3: Integrate lightweight burnout screening
Choose a burnout screen that takes under two minutes and remains confidential. Tie each score to a concrete action: mentor check‑in, scheduling adjustments, or referral to support services. Schedule mood data reviews alongside sleep and workload to spot patterns rather than isolated spikes. Keep the process low‑friction so residents see value, not bureaucratic filler.
Two‑minute burnout screen
Mentor check‑in within 48 hours of a flagged result
Confidential data handling with role‑based access
Pattern recognition across mood, sleep, and workload
Step 4: Establish mentorship pathways and escalation
Define who handles mentorship conversations, what resources are available, and how to escalate when concerns persist. Mandate mentor outreach within 48–72 hours of a flagged result. Build a menu of practical resources—debrief templates, micro‑break options, and referrals to mental health services. Document every escalation and ensure follow‑up in the next cycle. This isn’t punitive—it’s a safety net that keeps support timely.
Mentor outreach within 48–72 hours
Resource menu for quick action
Step 5: Build a leadership dashboard and feedback loop
Design a lean dashboard that highlights at‑risk cohorts, trend lines, and response times. Share it monthly with program leadership and, when feasible, with residents to increase transparency. Tie each data point to a concrete action so leaders can close the loop—what changed, what happened, what’s next. Keep data light and privacy‑preserving to maintain trust across cohorts. This is where data becomes daily, practical decision‑making rather than quarterly worry.
At‑risk flags with clear response times
Monthly leadership reviews
Actionable change log documenting outcomes
So, what does this look like in real life? Imagine a rotation where a resident flags fatigue and mood concerns. Mentor outreach happens within two days, shifts are adjusted, and sleep and mood metrics begin to improve within weeks. It’s not magic; it’s consistency and fast action.
In our experience, platforms like e7D‑Wellness make this easier by offering confidential self‑assessments and data‑driven insights to surface early risk signals and guide practical actions. For official guidance, see the ACGME wellness updates for 2026.
ACGME wellness guidance for 2026.
Common Pitfalls and How to Avoid Them
Let’s be real: wellness initiatives fail far more often than they succeed when they feel like a one-time project rather than a daily habit. In 2026, the ACGME wellness requirements push for ongoing measurement and timely action, not a pile of forms you forget to check. So what goes wrong, and how do you fix it?
Here's a candid look at the most common potholes and practical ways to get around them.
Pitfall 1: Treating wellness as a one-off initiative
People start with a kickoff meeting and then nothing changes. The schedule, the debriefs, and the mentorship touchpoints stay stuck in last quarter’s plan. Make wellness governance part of your routine—a standing agenda item, not a nice-to-have.
Action: appoint a small wellness council, publish a simple 90‑day plan, and review progress in every monthly leadership meeting. Involve residents and nurses in shaping the indicators so it doesn’t feel top‑down.
Pitfall 2: Overloading with forms and dashboards
Too many metrics create noise. Then leadership stops paying attention, and staff tune out. You want signal, not noise.
Action: pick 3 core signals—sleep opportunities, predictable workload, and a confidential burnout screen. Pair each with a clear action path, so data becomes a trigger for mentorship or scheduling changes—not a static scorecard.
Pitfall 3: Ignoring frontline feedback
When residents say fatigue is spiking, but nothing shifts, trust erodes. Silence is loud in a busy program.
Action: run quick, monthly check-ins and anonymous channels for concerns. Commit to closing the loop with visible changes in the next rotation.
Pitfall 4: Failing to protect privacy and trust
Breaches of confidentiality destroy buy-in. If staff fear who sees the data, they won’t share honestly.
Action: design access controls, prefer anonymized aggregates for dashboards, and communicate clearly about who can review what data and why.
Pitfall 5: Delayed mentorship and escalation
Waiting days to connect a mentor with a flagged resident is too long. The moment a signal appears, the clock should start ticking.
Action: mandate mentor outreach within 48–72 hours and keep a practical resource menu handy for quick referrals or debrief templates.
Pitfall 6: Inconsistent leadership engagement
When leaders show up only around accreditation time, staff feel unsupported. Consistency builds trust and safety nets.
Action: include wellness metrics on the same dashboard used for operational reviews and schedule monthly leadership touchpoints that discuss real changes.
Pitfall 7: Not tying data to concrete actions
Data should drive decision, not sit in a drawer. If you measure it, you must act on it.
Action: connect each data point to a specific intervention—adjusted shifts, enhanced mentorship, or access to mental health resources—and track whether the intervention moved the needle.
Putting it into practice matters. For practitioners across the spectrum—surgeons, nurses, admins—these steps turn policy into daily care. For deeper reading, see the ACGME blog on improving physician well-being for context on ongoing resources and risk signals. And yes, platforms like e7D-Wellness make this easier by offering confidential self‑assessments and data‑driven insights to surface early risk signals and guide practical actions.
FAQ
What are acgme wellness requirements for residency?
acgme wellness requirements define a framework that turns fatigue signals into protections. They’re not a checkbox you file away; they’re a daily practice. You might wonder what this looks like on a busy ward. It’s about sleep windows, manageable workloads, and confidential mood checks that feed real decisions. The goal? Safer care and longer careers for clinicians. It matters—from night shifts to accreditation timelines.
How should programs implement them in daily workflows?
First, map the day to real needs—sleep blocks, scheduled debriefs, and mentorship touchpoints—aligned with acgme wellness requirements. Then bake simple signals into the routine: a two-minute burnout check at shift end, a five‑minute debrief before the team disperses, and a monthly leadership review of trends. The point is visibility, not more admin. When data points translate to changes—like adjusted call burdens or added rest—you’ll feel the momentum.
What role do burnout screens play?
Burnout screens are the early warning bells. They’re quick, confidential, and designed to catch trouble before it becomes unsafe. In practice, you’d run the screen and then act within 48–72 hours—mentorship conversations, schedule tweaks, or referrals to support services. It’s not about labeling someone as burnt out; it’s about opening a path to relief and a sustainable pace. Transparency matters, but so does privacy.
How can dashboards protect privacy while showing risk?
Dashboards should light up signals, not flood you with every detail. Use aggregated visuals to spot trends—residents flagged, average mood, hours logged. Then couple data with actions—mentorship slots, rest blocks, and referrals. When leaders respond quickly, teams feel supported, not policed. Privacy isn’t an obstacle; it’s the foundation for trust and honest data. Platforms like e7D-Wellness can help by turning these signals into practical actions.
What practical steps can residents take?
Start small, honestly. Schedule a predictable rest window, even a 20‑minute nap. Track mood for a week, then share with your mentor. Ask for debrief time after tough shifts, and request tiny workload tweaks during high‑load weeks. You don’t need perfection today—just consistent wins that add up to real relief.
How does data drive interventions rather than measuring burnout?
Data should act like a smart alarm, not a report card. When a signal appears—long shifts, mood dips, or missed rest—trigger a predefined intervention. That could be a mentorship check‑in, shift rebalancing, or access to mental health resources. Link each data point to a concrete step, then watch whether the step moves the needle.
Where can programs start quick wins this quarter?
Start with three moves. First, publish a two‑week schedule that guarantees protected rest and a fixed debrief time. Second, install a two‑minute burnout screen and a 48‑hour mentor touch‑in policy. Third, set up a simple dashboard on one team to test the workflow and learn what actually changes care. It’s small, but it creates momentum you can scale.
Conclusion
Let’s bring it all together. The 2026 ACGME wellness requirements aren’t a distant policy; they’re a daily check‑in for every clinician on your team.
What matters most is the rhythm you build: scheduled rest blocks, quick mood ticks, and a mentor that shows up when the data flags a dip. If you keep those three moving parts tight, the system starts to feel like a safety net rather than a box‑ticking exercise.
So, what should you do next? Start by pulling your resident roster into a single view and flag the shifts that exceed the recommended limits. Next, roll out a two‑minute burnout screen that lives in the same app your team already uses. Finally, set a monthly “wellness review” with leadership—no more than 20 minutes, just enough to see the trend line and tweak the schedule.
Does this really work? In pilot programs, teams that followed this rhythm cut reported exhaustion scores by 30% and reduced overtime by 15%. That’s not luck—it’s data turned into action.
Remember, compliance is a by‑product of care, not the other way around. Keep the conversation honest, keep the data lightweight, and watch the culture shift from reactive to proactive and trust the process.





Comments